PTSD is not reserved for soldiers or military veterans, however; anyone who has experienced or witnessed a traumatic or life-threatening event, like a car or plane crash, torture, robbery, bombing or terrorist event, rape, murder, or any other violent situation, may be prone to developing PTSD.
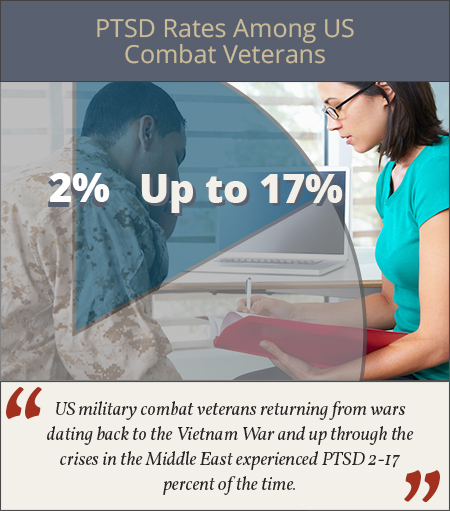 Commonly considered a concern mostly reserved for soldiers returning from war and military veterans, post-traumatic stress disorder, or PTSD, does affect this population at relatively high rates. According to the Australian and New Zealand Journal of Psychiatry, US military combat veterans returning from wars dating back to the Vietnam War and up through the crises in the Middle East experienced PTSD 2-17 percent of the time.
Commonly considered a concern mostly reserved for soldiers returning from war and military veterans, post-traumatic stress disorder, or PTSD, does affect this population at relatively high rates. According to the Australian and New Zealand Journal of Psychiatry, US military combat veterans returning from wars dating back to the Vietnam War and up through the crises in the Middle East experienced PTSD 2-17 percent of the time.
PTSD is not reserved for soldiers or military veterans, however; anyone who has experienced or witnessed a traumatic or life-threatening event, like a car or plane crash, torture, robbery, bombing or terrorist event, rape, murder, or any other violent situation, may be prone to developing PTSD. Most of the population in America has been through a traumatic event of some kind, the Journal of Traumatic Stress estimates almost 90 percent have, and just over 8 percent of the entire American adult population (as measured by an online sample in 2013) had suffered from PTSD in their lifetime. Women may battle PTSD at rates double those of men, according to Psych Central, and not everyone who goes through, or witnesses, a traumatic event will go on to develop PTSD.
PTSD is defined as a trauma-related, or stress-related disorder, according to the Diagnostic and Statistical Manuel of Mental Disorders – Fifth Edition (DSM-5), that is triggered by the direct exposure to a life-threatening situation, serious injury, sexual assault, or witnessing death or threat of death. When in a dangerous or life-threatening situation, the body and brain react by engaging the fight-or-flight reaction, which increases endorphins, speeds up central nervous system functioning, and heightens senses. In most cases, after the threat is over, the fear dissipates and bodily functions return to normal. In individuals with PTSD, this reaction is damaged, and they may continue to experience the fear reaction even when there is no longer a reason to be afraid or an imminent threat of danger.
 PTSD directly interferes with a person’s everyday life and ability to function at work, school, or home, and it is considered a mental health disorder. Much of the time, an individual battling PTSD may also abuse substances, perhaps as a coping mechanism, and addiction to drugs or alcohol and PTSD commonly co-occur. This means that an individual may have a dual diagnosis of both PTSD and substance use disorder at the same time. The U.S. Department of Veterans Affairs (VA) estimates that as many as two out of every 10 veterans who are suffering from PTSD also have substance use disorder (SUD). Both addiction and PTSD are treatable with integrated and specialized care plans.
PTSD directly interferes with a person’s everyday life and ability to function at work, school, or home, and it is considered a mental health disorder. Much of the time, an individual battling PTSD may also abuse substances, perhaps as a coping mechanism, and addiction to drugs or alcohol and PTSD commonly co-occur. This means that an individual may have a dual diagnosis of both PTSD and substance use disorder at the same time. The U.S. Department of Veterans Affairs (VA) estimates that as many as two out of every 10 veterans who are suffering from PTSD also have substance use disorder (SUD). Both addiction and PTSD are treatable with integrated and specialized care plans.
Onset of PTSD and Possibly Addiction
People often wonder why some people who experience a traumatic event develop PTSD while others do not. Some of this may be the result of genetic factors, or brain chemistry. The manner in which someone handles stress and stressful situations may be a factor. When someone is stressed, levels of serotonin, and other chemicals in the brain, may be affected. The prefrontal cortex and amygdala may also be affected, and these regions help to store memories and regulate moods and emotions. Sometimes these regions of the brain are not as developed or brain chemistry is not at the levels it should be, which may make someone more predisposed to PTSD or other mental health disorders, such as depression or anxiety. For instance, Psych Central reports that connections between certain brain regions, like the prefrontal cortex and the amygdala, may be weaker in someone with an anxiety disorder, making it more difficult for the person to regulate negative emotions.
 High levels of stress on a regular basis may actually change brain chemistry, leaving someone more susceptible to PTSD as a result of trauma. Younger individuals may also have underdeveloped brains, which could make them more liable to develop PTSD when exposed to trauma at a young age.
High levels of stress on a regular basis may actually change brain chemistry, leaving someone more susceptible to PTSD as a result of trauma. Younger individuals may also have underdeveloped brains, which could make them more liable to develop PTSD when exposed to trauma at a young age.
These same factors related to the development of PTSD may also be related to substance abuse patterns. Predisposition to developing PTSD, abusing substances, or developing an addiction may involve some of the same brain regions. Drugs and alcohol affect brain chemistry and the production of neurotransmitters that regulate mood and emotions, and suppress anxiety, fear, and depression. High levels of stress may then encourage someone to take drugs or drink alcohol in order to soothe these negative symptoms as a coping mechanism or a form of self-medication. PTSD symptoms may also be temporarily reduced with illicit drug or alcohol abuse.
Many drugs and alcohol increase some of the levels of endorphins or neurotransmitters in the brain, thus artificially increasing feelings of pleasure while decreasing the anxiety and depressive symptoms that may accompany PTSD. Individuals who suffer from PTSD may experience a drop in the levels of some of these brain chemicals as a result of the disorder, and drugs or alcohol may increase these chemical messengers temporarily, providing relief.
Abusing substances at a young age may also interfere with the development of the brain regions involving impulse control, mood regulation, and motivation, which can make it more likely for someone to develop substance use disorder, suffer from mental health disorders like PTSD, or both. It may be a kind of chicken-or-the-egg situation, as sometimes PTSD comes before substance abuse, which can lead to addiction, or addiction and substance abuse may make someone more susceptible to develop PTSD when exposed to a triggering event.
 Both substance abuse and PTSD interfere with the natural production of brain chemicals and change the way emotions and moods are regulated. Substance abuse may make people more likely to engage in risky behaviors that could put them in danger for involvement in a near-death or potentially fatal accident or dangerous situation. A study published in the European Journal of Psychotraumatology estimated that someone with PTSD was around three times more likely to also have substance use disorder than the rest of the general population.
Both substance abuse and PTSD interfere with the natural production of brain chemicals and change the way emotions and moods are regulated. Substance abuse may make people more likely to engage in risky behaviors that could put them in danger for involvement in a near-death or potentially fatal accident or dangerous situation. A study published in the European Journal of Psychotraumatology estimated that someone with PTSD was around three times more likely to also have substance use disorder than the rest of the general population.
Regardless of the cause, PTSD and substance abuse may complicate each other. Treatment for both disorders should be comprehensive and simultaneous, as each disorder may interfere with treatment for the other if ignored.
Signs and Symptoms of PTSD
There are four main subgroups of PTSD symptoms as highlighted by DSM-5:
- Avoidance symptoms: Reminders of a traumatic event can trigger negative emotions and avoidance symptoms, so someone may attempt to avoid these situations, places, people, or events that may trigger painful memories and may even change daily routines to do so. Avoidance symptoms include any difficult feelings, thoughts, or memories surrounding a traumatic event that may lead to a change in daily routine in an attempt to keep symptoms at bay.
- Re-experiencing symptoms: These symptoms may disrupt an individual’s daily life. They can pop up without warning and may be triggered in many different ways, including little things that may remind someone of the trauma. Re-experiencing symptoms include flashbacks, terrifying thoughts, reoccurring nightmares, and emotional distress.
- Arousal symptoms: Arousal symptoms are not necessarily triggered by a memory or reminder of a traumatic event, but instead may be constantly present in someone battling PTSD. Aggression, self-destructive or risky behavior, trouble sleeping, anger, irritability, feeling “on edge,” hyper vigilance, and being easily startled may all be symptoms of arousal or hyperarousal following an traumatic event. When these symptoms continue for a period of time, they are often linked to PTSD.
- Negative mood and cognition symptoms: There are a number of negative thoughts and moods associated with PTSD, including feeling numb emotionally, depression, extreme worry, guilt, short-term memory loss surrounding the trauma, lack of interest in activities that may have been previously enjoyed, self-blame or blame of others, and withdrawing from friends and family.
To be diagnosed with PTSD, someone generally experiences at least one symptom from each of the categories of symptoms for a period of 30 days or more, the National Institute of Mental Health (NIMH) reports. Symptoms may not appear right away either, but rather a few days or weeks may go by before someone starts to have PTSD symptoms after being involved in or witnessing a traumatic event. PTSD symptoms affect personal relationships, work and school output, and make everyday life tasks seem difficult to manage.
Correlation of PTSD and Addiction Symptoms
Just as PTSD may lead to addiction, and addiction may predispose someone to developing PTSD, some of the symptoms of PTSD may be similar to signs of addiction. Addiction is a disorder with both physical and mental components. Some of the emotional side effects may be similar to PTSD symptoms, such as social withdrawal, lack of desire to participate in activities that were enjoyed in the past, trouble sleeping, aggression, trouble regulating moods or emotions, short-term memory loss, inability to feel pleasure, guilt, depression, and self-destructive or risky behaviors.
Addiction may also interfere with daily life as individuals addicted to drugs or alcohol may not be able to fulfill school, family, or work obligations; as a result, they may experience a drop in production at school or work and difficulties with interpersonal relationships. Those addicted to drugs or alcohol are likely to spend the majority of their time using, recovering from, and looking for their next fix. Because of this, they may have financial, legal, or even criminal problems related to their substance abuse. Those with drug or alcohol problems may continue to abuse substances regardless of any social, emotional, physical, or other negative consequences. They may do so in physically dangerous situations and be unable to stop or reduce their substance abuse.
Substance abuse can interfere with treatment for PTSD. The journal Neurobiology of Learning and Memory reported that nicotine, alcohol, and cocaine in particular may affect some of the same regions of the brain involved in memory storage and the fear response that may be negatively impacted by PTSD, thereby making it more difficult to treat the disorder while abusing these substances. Drugs and alcohol can also make PTSD symptoms worse and often create bigger problems instead of providing relief.
 Combat and military veterans commonly experience PTSD and co-occurring substance abuse. Between 2004 and 2006, approximately 79 percent of the military members who had been involved in the Iraq/Afghanistan conflicts and seen in outpatient PTSD clinics were diagnosed with the disorder, while 20 percent also abused alcohol and 6 percent abused drugs, Psychiatric Times reported.
Combat and military veterans commonly experience PTSD and co-occurring substance abuse. Between 2004 and 2006, approximately 79 percent of the military members who had been involved in the Iraq/Afghanistan conflicts and seen in outpatient PTSD clinics were diagnosed with the disorder, while 20 percent also abused alcohol and 6 percent abused drugs, Psychiatric Times reported.
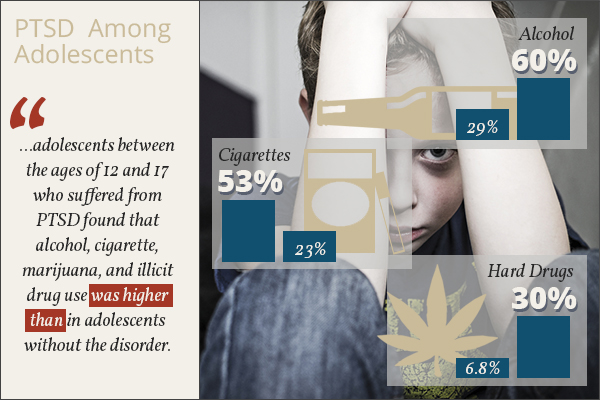
PTSD and comorbid substance abuse are also common in the general population, and young children and adolescents may be at a particularly high risk. One 2005 study of children and adolescents between the ages of 12 and 17 who suffered from PTSD found that alcohol, cigarette, marijuana, and illicit drug use was higher than in adolescents without the disorder. The Journal of Clinical Child Adolescent Psychology reported that of those surveyed, over 53 percent had used cigarettes and nearly 60 percent had abused alcohol in their lives compared to just over 23 percent lifetime use of cigarettes and over 29 percent lifetime alcohol use in those without PTSD. A quarter with PTSD used marijuana in their lives (not just experimentally) as opposed to just over 8 percent of those who didn’t have PTSD. Almost 30 percent of adolescents with PTSD had experimented with hard drugs in their lives compared to 6.8 percent of kids the same age without PTSD.
Types of Treatment for PTSD, Addiction, and Comorbid Disorders
A strong support system and healthy ways to cope with stress are both helpful in preventing substance abuse and PTSD, and work well in treatment of both disorders. Cognitive Behavioral Therapy (CBT) is a type of therapy that generally uses both group and individual sessions to work on changing negative behaviors and thoughts into more positive ones, teaching coping mechanisms and identifying potential triggers and how to handle them as they arise. Anxiety and depression may both be byproducts of PTSD and substance abuse, and they can be minimized with CBT methods.
 Many support groups exist for PTSD, substance abuse, and co-occurring disorders, and these groups can provide an outlet where people understand what someone might be going through and can offer a sympathetic ear. Families and couples may attend therapy or support groups together to mend damage within personal relationships. Exposure therapy is another form of PTSD treatment that introduces creative methods, such as writing or pictures, to expose individuals to their fears or traumatic memories in a safe and nonthreatening manner in order to learn how to face and overcome them.
Many support groups exist for PTSD, substance abuse, and co-occurring disorders, and these groups can provide an outlet where people understand what someone might be going through and can offer a sympathetic ear. Families and couples may attend therapy or support groups together to mend damage within personal relationships. Exposure therapy is another form of PTSD treatment that introduces creative methods, such as writing or pictures, to expose individuals to their fears or traumatic memories in a safe and nonthreatening manner in order to learn how to face and overcome them.
Medications are often used to treat withdrawal symptoms from substances of abuse and also to treat PTSD symptoms. When someone is dependent on a drug or alcohol, physical and emotional side effects can occur while the substance leaves the body, as the brain attempts to regulate itself. These withdrawal symptoms may include nausea and vomiting, sweats, chills, tremors, trouble sleeping, depression, anxiety, confusion, cravings, cognitive difficulties, and mood swings. In some cases, withdrawal can be a life-threatening process if not managed correctly. Most often, and especially in cases of withdrawal from alcohol, benzodiazepines, and opiates, medical detox is recommended. This takes place in a specialized treatment facility that provides 24-hour medical monitoring and may involve the use of medications to reduce specific symptoms.
When people suffer from PTSD, the detox process can be more complex. In these cases, withdrawal from drugs or alcohol should be even more carefully and professionally managed to minimize potential side effects.
 NIMH states that the U.S. Food and Drug Administration (FDA) currently approves two antidepressant medications for the treatment of PTSD: sertraline (Zoloft) and paroxetine (Paxil). These medications help with symptoms of sadness and emotional numbness, and they can regulate emotions and help to prevent suicidal ideations as well. Anti-anxiety medications, like benzodiazepines, other antidepressants, and antipsychotics, may also be prescribed in some cases. However, when an individual has a history of abusing substances or addiction, medical professionals may decide against certain medications that may be habit-forming, such as benzodiazepines and some antidepressants. It is important therefore that all treatment providers be on the same page, when helping someone with a dual diagnosis of PTSD and addiction, to ensure that all treatments and medications are safe and working toward the same goals.
NIMH states that the U.S. Food and Drug Administration (FDA) currently approves two antidepressant medications for the treatment of PTSD: sertraline (Zoloft) and paroxetine (Paxil). These medications help with symptoms of sadness and emotional numbness, and they can regulate emotions and help to prevent suicidal ideations as well. Anti-anxiety medications, like benzodiazepines, other antidepressants, and antipsychotics, may also be prescribed in some cases. However, when an individual has a history of abusing substances or addiction, medical professionals may decide against certain medications that may be habit-forming, such as benzodiazepines and some antidepressants. It is important therefore that all treatment providers be on the same page, when helping someone with a dual diagnosis of PTSD and addiction, to ensure that all treatments and medications are safe and working toward the same goals.
Holistic methods may also help. For example, yoga and meditation can be great ways to learn how to deal with stress and anxiety in a safe and effective manner. Alternative methods like these can discourage the return of PTSD symptoms and decrease the perceived need to abuse substances as an escape. Maintaining a structured schedule, with set meal and sleeping times, can help reset the body and keep systems balanced. Quality sleep and well-balanced meals improve a person’s physical health and, in turn, can enhance their overall wellbeing.
With cases of co-occurring disorders, it’s important that all conditions are treated in a comprehensive manner. There is hope in recovery for those suffering from co-occurring addiction and PTSD. A treatment center that is equipped to offer both substance abuse and mental health treatment can provide the care needed for full recovery from both issues.
Get Help Now.
Has addiction stolen your loved one? Take action and call (619) 577-4483 or fill out this form to speak with a Treatment Consultant about our drug rehab center or one of our facilities across the United States.
