California Alcoholism Rates, Treatment, and Statistics
California is the one of the largest states by area and has the biggest population out of all 50 states, with 38.8 million residents (at last count in 2014).[1] With a highly diverse population and various ethnic, age, social, and economic demographics represented, one of the common denominators among many Californians may be alcohol, drug, and mental health concerns, which are nondiscriminatory and can affect anyone.
Alcohol is considered the most used and abused mind-altering and potentially addictive substance in America. One out of every 12 adults is thought to have an alcohol dependence or abuse concern.[2] Between 2005 and 2009, over half of Californians, aged 12 and older, reported drinking alcohol in the past 30; this rate was similar to national averages.[3] Drinking alcohol is not generally considered an issue, as it is a legal substance for those over age 21, inexpensive, readily available, a part of many socially acceptable situations, and may even have some health benefits. Binge or heavy drinking patterns may create issues that may include the development of an alcohol abuse or dependence problem, however.
Binge Drinking Rates Increasing in California

Binge drinking is when a man drinks more than five drinks in about a two-hour period, or a woman drinks four in the same time period, and the blood alcohol concentration (BAC) is raised above 0.08 g/dL. Heavy drinking is binge drinking (or having five or more drinks in a sitting) five or more times a month.[4] About a quarter of the American adult population binge drank in the month prior to a national survey in 2013, and binge drinking is the most frequent method of excessive alcohol consumption in the nation.[5], [6] Californians, in 2012, binge drank at rates similar to the national average, although binge drinking does seem to be on the rise within the state.[7]
Traditionally, men may be as much as twice as likely to binge drink than women, and affluent individuals making $75,000 or more annually are more likely to binge drink.[8] It may be becoming more socially acceptable for woman to drink more across the nation in general and in California specifically. Coupling that with the influx of tech jobs and wealthy professionals in the greater Bay Area, it may not be surprising that Santa Clara County, along with San Francisco, Alameda, Santa Cruz, and San Mateo Counties saw increases in binge drinking rates in the 10-year span from 2002 to 2012.[9]
Bars and establishments serving alcohol that are close together may increase binge drinking rates, as may weak alcohol control policies that control how, when, and where alcohol can be sold. Alcohol abuse and binge drinking may also be common in the underprivileged Californian population as well as those more well-off population, perhaps as an escape valve. Whatever the reason, overall, California residents engaging in episodes of binge drinking rose almost 30 percent in 2012 over rates measured in 2002 and may continue to increase.[10]
In California, the rate of residents over the age of 11 who were considered to suffer from an alcohol abuse or dependency in 2012-2013 was slightly higher than the national average at 7.3 percent as compared to 6.7 percent.[11] Approximately 2.3 million California residents, per year between the years 2009 and 2013, battled alcohol use or dependence, or an average of 7.5 percent of the population aged 12 and older.[12]
Alcohol abuse and dependency can create a plethora of social, emotional, physical, legal, and economic problems. In 2006, excessive alcohol use was estimated to cost the state of California close to $32 billion, which was the fifth highest cost per capita among US states.[13] Costs to society count lost workplace production, legal costs, criminal justice expenses, and healthcare costs, meaning that in 2006, one drink cost the California economy $2.44 or $1,165 per capita.[14]
Alcoholism is considered to be a treatable disease. Fortunately, California offers its residents a range of mental health and substance abuse services to choose from.
California’s Substance Abuse Services
Between 2009 and 2013, approximately 186,000 people in California were treated for each year for alcohol dependence or abuse, which was only about 8 percent of those who needed treatment.[15] In 2012, in Los Angeles County, alcohol was the second most commonly cited drug of abuse for individuals admitted to public treatment programs at 23 percent of all admissions behind only marijuana.[16] In general, across California, for the fiscal year (FY) 2009/2010, marijuana jumped ahead of alcohol treatment admissions for the first time, since before 2005 at least. Treatment admissions for both were behind methamphetamine when detox services were excluded.[17]
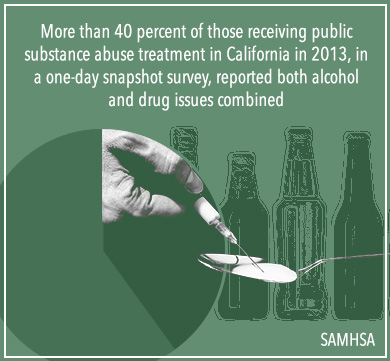
In the case of detox treatment, alcohol public treatment admissions were second only to heroin for the FY 2009/2010.[18] Drugs and alcohol are commonly mixed, however, and individuals may battle issues with more than one substance at a time. More than 40 percent of those receiving public substance abuse treatment in California in 2013, in a one-day snapshot survey, reported both alcohol and drug issues combined, while only just below 17 percent reported problems with alcohol on its own.[19]
Both private and public treatment options are likely to provide a range of necessary services, such as:
- Detox services
- Medical detox
- Emergency counseling and crisis services
- Co-occurring disorders treatment
- Intensive outpatient treatment programs
- Preventative programs and services
- Educational offerings
- Outpatient treatment
- Pharmacological and behavioral treatments
- Residential treatment programs
- Special programs for women and children
- Driving under the influence (DUI) programs
- Programs for specialty populations
- Alternative or complementary methods
- Transitional care
- Family programs
- Recovery services
There are two main forms of substance abuse treatment within California: public treatment services that are provided through the California Department of Health Care Services (DHCS) and private treatment options offered by privately funded facilities.[20]
Generally speaking, public programs are funded by the state and provide services to all residents, either for low-cost or free of charge, depending on a person’s economic status. In California, public treatment is provided at a county level, and a County Directory provides telephone numbers of the local offices.[21] Public providers may accept Medi-Cal (which is California’s Medicaid program) recipients, and usually individuals will start the treatment process by first visiting a primary care physician and receiving a referral to a treatment program.[22]
Private programs are typically considered fee-for-service providers and may accept insurance for payment. Private programs may not require a referral first, and generally, an evaluation and assessment are done initially to help families and loved ones choose a program that will best suit their needs. In order to provide substance abuse treatment or recovery services within the state of California, both private and public providers must be licensed through DHCS, and a directory of licensed providers by county can be found here.[23]
California Treatment Provider Specifications
To be certified as a drug or alcohol abuse counselor in the state of California, individuals must go through one of three accredited organizations recognized by DHCS and certified through National Commission of Certified Agencies (NCCA): the Addiction Counselor Certification Board of California, which is affiliated with the California Association for Alcohol/Drug Educators (CAADE); the California Consortium of Addiction Programs and Professionals (CCAPP); and the California Association of DUI Treatment Programs (CADTP).[24]
CCADE Certifications:
- Certified Addiction Treatment Counselor (CATC): complete at least 21 units (315 hours) in a CAADE-certified addiction studies program at a CAADE accredited college or a private post secondary school, 2,240 hours of supervised employment in a state licensed substance abuse facility, and pass the CATC exam
- CATC I: complete CAADE-accredited addiction studies program at a regionally accredited university or college, 2,240 hours of supervised employment in a state licensed substance abuse facility, and pass the CATC exam
- CATC II: earn an associate’s degree (AA) and complete a CAADE-accredited addiction studies program, 2,240 hours of supervised employment in a state-licensed substance abuse facility, and pass the CATC exam
- CATC III: earn a bachelor’s degree in alcohol and drug studies or a related field, complete 15 units of a CAADE-accredited addiction studies program including two internship courses, 2,240 hours of supervised employment in a state-licensed substance abuse facility, and pass the CATC exam
- CATC IV: earn a master’s degree in alcohol and drug studies or a related field, complete 15 units of a CAADE-accredited addiction studies program including two internship courses, 2,240 hours of supervised employment in a state-licensed substance abuse facility, and pass the CATC exam
- CATC V: earn a doctorate in alcohol and drug studies or a related field, complete 15 units of a CAADE-accredited addiction studies program, 2,240 hours of supervised employment in a state-licensed substance abuse facility, and pass the CATC exam
- CATC (I,II, III, IV, V) N: earn a nursing degree in a related field, complete 15 units of a CAADE-accredited addiction studies program including two internship courses, 2,240 hours of supervised employment in a state-licensed substance abuse facility, and pass the CATC exam[25]
- Registered Alcohol Drug Technician I (RADT-I): complete a nine-hour orientation course on ethics, CCAPP application, and sign code of conduct and scope of practice forms
- RADT- II: complete 315 hours of substance abuse disorder (SUD) specific education, 255-hour field practicum, and pass ICRC written exam; requires renewal every two years and continuing education
- Certified Alcohol Drug Counselor – Certified Addiction Specialist (CADC- CAS): 155 hours of SUD specific education, 255-hour field practicum, 160-hour internship, pass ICRC written exam, and 2,080 hours of work experience; requires renewal every two years and continuing education
- CADC I: complete 315 hours Alcohol and Other Drug (AOD) specific education, 255-hour field practicum, pass ICRC written exam, and 4,000 hours work experience; requires renewal every two years and continuing education
- CADC II: complete 315 hours Alcohol and Other Drug (AOD) specific education, 255-hour field practicum, pass ICRC written exam, 6,000 hours work experience of which 2,000 hours may be substituted for an associate degree (AA) in SUD or Allied Mental Health Profession (AMHP); requires renewal every two years and continuing education
- CADC Clinical Supervisor (CADC- CS): must complete all requirements of CADC II or have a bachelor’s degree in SUD/AMHP, 6,000 hours of supervised training, 2,000 hours of SUD counseling experience, 40 hours of didactic training in clinical supervision, and pass the ICRC Clinical Supervisor Written Exam
- Licensed Advanced Alcohol Drug Counselor (LAADC): earn a master’s degree in SUD/AMHP, which includes 180 hours of SUD-specific courses and six hours of ethics, 2,700 hours of SUD counseling experience, 10 hours working in private practice, 20 hours of clinical supervision, 20 hours of co-occurring disorder education, and pass the ICRC Advanced Alcohol Drug Counselor written exam[26]
There are also specialty certifications, credentials, and endorsements a provider can receive on top of these certifications that include: Certified Criminal Justice Professional (CCJP), Certified Co-Occurring Disorder Professional (CCDP), Certified Peer Recovery Specialist (CPRS), California Certified Prevention Specialist (CCPS), Sober Living Specialist (SLS), Certified Recovery Program Manager (CRPM), Intervention Specialist (IS), Women’s Treatment Specialist (WTS), and Medication-Assisted Treatment Specialist (MATS).[27] All of these have additional requirements.
- CADTP Alcohol/Other Drug Counselor (CAODC): must complete 155 hours in formal education on drug and alcohol abuse, 160 hours of supervised training, 2,080 hours of substance abuse counseling experience, register with CADTP, and pass a written exam
- CADTP Alcohol/Other Drug Counselor – Advanced (CAODC-A): complete 350 hours of formal classroom education on drug and alcohol abuse and have five years of experience working as a substance abuse counselor
- CADTP Alcohol/Other Drug Counselor – Clinical Supervisor (CAODC-CS): complete either 450 hours of formal classroom education on drug and alcohol abuse or a CADTP-A, five years of clinical experience as a substance abuse counselor or 10,000 hours of general clinical experience, two years as a clinical supervisor, and 40 hours of clinical supervisor education
- Reciprocity: for applicants with current certifications from organizations who were previously approved to provide certification through DHCS or meet specific criteria[28]
Other professionals who may treat addiction or mental health concerns may include medical and mental health care providers like doctors, nurses, medical technicians, nurse practitioners, psychologists, psychiatrists, and complementary medicine providers to name a few.
Call Now (619) 577-4483
Negative Effects of Alcohol and Untreated Addiction
 Alcohol was involved in 88,600 deaths in 2010 in America and costs society upwards of $220 billion annually.[29] Data from 2006 suggests that 10 percent of the national alcohol-related fatalities were Californians, as 10,000 people died from alcohol-related causes while another 72,000 were hospitalized.[30]
Alcohol was involved in 88,600 deaths in 2010 in America and costs society upwards of $220 billion annually.[29] Data from 2006 suggests that 10 percent of the national alcohol-related fatalities were Californians, as 10,000 people died from alcohol-related causes while another 72,000 were hospitalized.[30]
Like with other drugs, a person can overdose on alcohol. Between 2010 and 2012, six people died in the United States every day from alcohol poisoning, and around 300 people died in California each year as the result of a toxic buildup of alcohol in the body that could not be broken down successfully.[31], [32] Shallow breathing, vomiting, seizures, trouble remaining conscious, and low body temperatures are all signs of alcohol poisoning, and immediate medical attention should be sought. Alcohol dependency is often the result of repeated patterns of excessive alcohol abuse and may raise the risk for an alcohol poisoning fatality. Alcohol dependence plays a role in about 30 percent of alcohol poisoning deaths.[33]
Excessive or prolonged alcohol abuse can cause a multitude of physical health problems resulting in disease, injury, or even death. Between 2006 and 2009 in California, emergency department (ED) visits involving alcohol were twice as common as those involving drugs, and 280 people per 100,000 were treated in an ED for alcohol-related causes in 2009.[34] Hospitalizations where the principle diagnosis involved alcohol, between 2005 and 2009, were also higher than drug-related hospitalizations at 95.2 per 100,000 as opposed to 79.3 per 100,000.
The most common hospital discharge diagnosis involving alcohol was alcohol-related psychosis followed by alcohol dependence and alcoholic liver disease.[35] Alcohol-related psychosis is often the result of alcohol withdrawal, which can be life-threatening and should be considered a medical emergency. Long-term alcohol abuse and alcoholism left untreated can wreak havoc on a person’s brain and body and may be a contributing factor to developing liver disease, heart or cardiovascular problems, cancer, diabetes, gastrointestinal problems, sexually transmitted diseases, gout, dementia, and more.
The Impact of Alcohol on Crime Rates
Alcohol decreases a person’s inhibitions and impulse control functions, as well as impairs a person’s decision-making abilities, reaction time, and motor coordination, which may result in injury or in being in a hazardous or criminal situation. In 2007, approximately 14,555 Californians were treated in an ED for a non-fatal motor vehicle crash in which alcohol was a contributing factor. In 2009, there were 1,263 alcohol-involved car crash fatalities in California.[36] Males between the ages of 26 and 34 were involved and treated in EDs most often in the automobile accidents involving alcohol and impaired driving in California in 2007.
In 2013, there were 160,388 arrests for driving under the influence, or DUI, with the average arrestee having a BAC of twice the legal limit at the time of their arrest.[37] Almost a quarter of these arrests were in Los Angeles County, and close to half of all the DUI arrests in California occurred within the counties of Orange, San Diego, Los Angeles, and San Bernardino in 2013.[38]
When people are suspected of driving under the influence in California, they may be asked to take a chemical test by an arresting officer. If the test is refused, it will result in a one-year suspension of their driver’s license. If the person is 21 or older and fails the test, their license will be suspended for at least four months for the first offense. Multiple offenders may be looking at a minimum of a year’s suspension and those under the legal drinking age may as well.[39] A DUI conviction may also result in jail time, fines, or additional criminal penalties.
The majority of alcohol arrests in California (based on 2009 data) are for DUI, public intoxication, or a liquor law violation, and all are considered misdemeanors.[40] Alcohol may also contribute to the perpetuation of other crimes or violent acts that may have stricter penalties and be more serious offenses. Sexual assault, homicide, spousal abuse, child neglect or abuse, and other violent acts may be escalated and their risk factors increased by the presence of alcohol. It is estimated that in between 32 and 50 percent of all homicides the person was drinking before committing the act, and two-thirds of those who fall victim to intimate violence report that the perpetrator was drinking at the time.[41] It is estimated that around 40 percent of women in California will be involved in physical intimate partner violence at some point in their lifetime, and three-quarters of those who do are likely to have minor children living at home at the time. In 2012 there were close to 160,000 calls to law enforcement agencies for domestic violence in California.[42]
Alcoholism and Mental Health
 Alcohol is a psychoactive substance that may temporarily dull emotional pain and memory of trauma, and increase pleasure. Over time, alcohol abuse can change the brain’s chemical makeup, and it may become harder for an individual dependent on alcohol to feel pleasure without drinking. The individual may even become depressed and irritable when without alcohol.
Alcohol is a psychoactive substance that may temporarily dull emotional pain and memory of trauma, and increase pleasure. Over time, alcohol abuse can change the brain’s chemical makeup, and it may become harder for an individual dependent on alcohol to feel pleasure without drinking. The individual may even become depressed and irritable when without alcohol.
Alcohol abuse may be the result of an attempt to self-medicate troubling emotions or mental illness symptoms, but may actually result in making them worse in the long run. It is estimated that mental illness and alcohol abuse or dependence co-occur around a third of the time.[43] This may increase the risk for suicidal behaviors or thoughts. In California between 2009 and 2013, around 1 million adults aged 18 or older had serious thoughts of suicide each year.[44] In 2009, approximately 3,760 Californians committed suicide, and 16,554 suffered from a self-inflicted injury that was nonfatal.[45]
Californians seem to suffer from mental illness and depression at rates similar to the average American, which may be exacerbated by the abuse or dependence of alcohol.[46] When an individual battles both depression, or any mental illness, and substance abuse, the optimal treatment program will be an integration between both medical and mental health resources. Programs that focus on the treatment of co-occurring disorders may be highly beneficial.
Local Substance Abuse and Mental Health Resources
An estimated 63.5 percent of Californians aged 18 or older needing treatment or counseling for mental health concerns did not receive what they needed between 2009 and 2013. More than 70 percent of the 1.8 million each year who did receive public mental health services reported that it helped them and improved their ability to function.[47]
There is often a treatment gap between those needing services and those receiving them. There may be many perceived barriers to treatment, such as cost, accessibility, knowledge of treatment options, and lack of healthcare coverage. There is a wealth of public and private organizations in California that strive to close this treatment gap by providing information and services to residents for mental health concerns, substance abuse, or both.
Below is a list of California mental health and substance abuse resources:
- Mental Health Substance Use Disorder Services (MHSUDS) through the California DHCS[48]
- Directories for Substance Use Disorder Services through the California DHCS[49]
- Mental Health 24-hour Crisis Hotlines by County through California DHCS[50]
- National Alliance on Mental Illness (NAMI) California, with 71 local affiliates to help educate the public and provide mental health support[51]
- Behavioral Health Services Treatment Locator Tool provided by the Substance Abuse and Mental Health Services Administration (SAMHSA)[52]
- Alcoholics Anonymous (AA) list of local resources by city[53]
Each individual county in California has region-specific resources available to help families and loved ones struggling with alcohol abuse and/or mental illness as well. Nonprofit and community organizations may provide preventative and educational measures as well as information on local treatment options.
Alcoholism and mental health can both be improved with treatment. There are numerous substance abuse and behavioral health services of all types within the state of California for residents to choose from. Families are sure to find one that will fit all of their specific needs to provide a healthy foundation for a lasting recovery.
Citations
[1] (Dec. 2014). “Florida Surpasses New York to Become the Nation’s Third Most Populous State, Census Bureau Reports.” United States Census Bureau. Accessed November 30, 2015.
[2] (2015). “Facts About Alcohol.” National Council on Alcoholism and Drug Dependence, Inc. (NCADD). Accessed November 30, 2015.
[3] (n.d.) “Indicators of Alcohol and Drug Abuse FY 2010-11.” California Department of Alcohol and Drug Programs (ADP). Accessed November 30, 2015.
[4] (n.d.). “Alcohol Facts and Statistics.” National Institute on Alcohol Abuse and Alcoholism (NIAAA). Accessed November 30, 2015.
[5] Ibid.
[6] (Oct. 2015). “Fact Sheets: Binge Drinking.” Centers for Disease Control and Prevention (CDC). Accessed November 30, 2015.
[7] Ostrov, B.F. (April 2015). “Silicon Valley, Bay Area See Huge Rise in Binge Drinking.” Santa Cruz Sentinel. Accessed November 30, 2015.
[8] (Oct. 2015). “Fact Sheets: Binge Drinking.” Centers for Disease Control and Prevention (CDC). Accessed November 30, 2015.
[9] Ostrov, B.F. (April 2015). “Silicon Valley, Bay Area See Huge Rise in Binge Drinking.” Santa Cruz Sentinel. Accessed November 30, 2015.
[10] Ibid.
[11] (2015). “Behavioral Health Barometer, California 2014.” Substance Abuse and Mental Health Services Administration (SAMHSA). Accessed November 30, 2015.
[12] Ibid.
[13] (Nov. 2014). “Alcohol Abuse and Health.” Centers for Disease Control and Prevention (CDC). Accessed November 30, 2015.
[14] Ibid.
[15] (2015). “Behavioral Health Barometer, California 2014.” Substance Abuse and Mental Health Services Administration (SAMHSA). Accessed November 30, 2015.
[16] Brecht, M. Ph.D. (Nov. 2013). “Drug Abuse Patterns and Trends in Los Angeles County, California: June 2013.” National Institute on Drug Abuse (NIDA). Accessed November 30, 2015.
[17] (n.d.) “Indicators of Alcohol and Drug Abuse FY 2010-11.” California Department of Alcohol and Drug Programs (ADP). Accessed November 30, 2015.
[18] Ibid.
[19] (2015). “Behavioral Health Barometer, California 2014.” Substance Abuse and Mental Health Services Administration (SAMHSA). Accessed November 30, 2015.
[20] (2015). “Substance Use Disorder Services- Alcohol and Other Drugs Programs.” California Department of Health Care Services (DHCS). Accessed November 30, 2015.
[21] (2015). “Alcohol and Other Drugs Programs County Directory.” California Department of Health Care Services (DHCS). Accessed November 30, 2015.
[22] (2015). “Drug Medi-Cal (DMC) Treatment Program.” California Department of Health Care Services (DHCS). Accessed November 30, 2015.
[23] (July 2015). “Department of Health Care Services Licensing and Certification Section Status Report.” California Department of Health Care Services (DHCS). Accessed November 30, 2015.
[24] (2015). “Counselor Certification Organizations.”California Department of Health Care Services (DHCS). Accessed November 30, 2015.
[25] (n.d.). “CATC Tiers.” California Association for Alcohol/Drug Educators (CAADE). Accessed November 30, 2015.
[26] (n.d.). “CCAPP Career Ladder.” California Consortium of Addiction Programs and Professionals (CCAPP). Accessed November 30, 2015.
[27] Ibid.
[28] (n.d.). “Certification as an Alcohol and Other Drug Abuse Counselor (CAODC).” California Association of DUI Treatment Programs (CADTP). Accessed November 30, 2015.
[29] Ostrov, B.F. (April 2015). “Silicon Valley, Bay Area See Huge Rise in Binge Drinking.” Santa Cruz Sentinel. Accessed November 30, 2015.
[30] Simon, M., Stahre, M. (2010). “Alcohol-Related Deaths and Hospitalizations by Race, Gender, and Age in California.” The Open Epidemiology Journal. Accessed November 30, 2015.
[31] (Jan. 2015). “Vital Signs.” Centers for Disease Control and Prevention (CDC). Accessed December 1, 2015.
[32] Aleaziz, H. (Jan. 2015). “CDC: 300 Die Yearly in California from Alcohol Poisoning.” SF Gate. Accessed December 1, 2015.
[33] (Jan. 2015). “Vital Signs.” Centers for Disease Control and Prevention (CDC). Accessed December 1, 2015.
[34] (n.d.) “Indicators of Alcohol and Drug Abuse FY 2010-11.” California Department of Alcohol and Drug Programs (ADP). Accessed November 30, 2015.
[35] Ibid.
[36] (n.d.) “Indicators of Alcohol and Drug Abuse FY 2010-11.” California Department of Alcohol and Drug Programs (ADP). Accessed December 1, 2015.
[37] (2015). “Annual Report of the California DUI Management Information System.” California Department of Motor Vehicles (DMV). Accessed December 1, 2015.
[38] Ibid.
[39] (2011). “Arrest for Driving Under the Influence DUI General Information.” California Department of Motor Vehicles (DMV). Accessed December 1, 2015.
[40] (n.d.) “Indicators of Alcohol and Drug Abuse FY 2010-11.” California Department of Alcohol and Drug Programs (ADP). Accessed December 1, 2015.
[41] (April 2006). “Alcohol and Violent Crime: What is the Connection? What Can be Done?” The National Center for Alcohol Law Enforcement Pacific Institute for Research and Evaluation. Accessed December 1, 2015.
[42] (n.d.). “The Facts: Domestic Violence in California.” The California Partnership to End Domestic Violence. Accessed December 1, 2015.
[43] (n.d.). “Dual Diagnosis.” National Alliance on Mental Illness (NAMI). Accessed December 1, 2015.
[44] (2015). “Behavioral Health Barometer, California 2014.” Substance Abuse and Mental Health Services Administration (SAMHSA). Accessed December 1, 2015.
[45] (2009). “Data Summary Sheet On Suicide Deaths And Nonfatal Self-Inflicted Injuries California Statewide.” California Department of Mental Health Office of Suicide Prevention. Accessed December 1, 2015.
[46] (2015). “Behavioral Health Barometer, California 2014.” Substance Abuse and Mental Health Services Administration (SAMHSA). Accessed December 1, 2015.
[47] Ibid.
[48] (n.d.). “(MHSUDS) Mental Health Substance Use Disorder Services.” California Department of Health Care Services (DHCS). Accessed December 1, 2015.
[49] (n.d.) “Directories for Substance Use Disorder Services.” California Department of Health Care Services (DHCS). Accessed December 1, 2015.
[50] (Dec. 2012). “Local County Mental Health 24-Hour Crisis Intervention Numbers.” .” California Department of Health Care Services (DHCS). Accessed December 1, 2015.
[51] (2011). “NAMI California Mission.” NAMI California. Accessed December 1, 2015.
[52] (n.d.). “Behavioral Health Treatment Locator.” Substance Abuse and Mental Health Services Administration (SAMHSA). Accessed December 1, 2015.
[53] (2015). “A.A. Near You.” Alcoholics Anonymous (A.A.). Accessed December 1, 2015.
